Combination Therapy for AMD Fails to Improve Vision Versus Single Drug
LONG BEACH, Calif. — Outcomes in neovascular age-related macular degeneration (nAMD) failed to improve with the addition of a multitargeted trap fusion protein to anti-VEGF therapy, according to a randomized trial reported here.
After a year of treatment, improvement in best corrected visual acuity (BCVA) averaged 13.66 EDTRS letters with aflibercept (Eylea) alone and 12.82 and 13.48 letters, respectively, with aflibercept plus two dosing schedules of sozinibercept. Secondary BCVA-associated endpoints also did not improve with the addition of the endothelin inhibitor, nor did changes in central subfield thickness (CST).
Unblinded results from a phase III trial comparing ranibizumab (Lucentis) with or without sozinibercept also showed no improvement in key outcomes with the endothelin antagonist, reported Charles Wykoff, MD, PhD, of Retina Consultants of Texas in Houston, at the American Society of Retina Specialists meeting.
“I think, first and foremost, this just shows that our current therapeutics…are incredibly effective agents,” said Wykoff. “The bar is set incredibly high to improve outcomes in exudative retinal diseases.”
During a discussion that followed the presentation, Rahul Khurana, MD, of Northern California Retina Vitreous Associates in San Mateo, pointed out the “really impressive phase II data” with sozinibercept, and asked, “Do you have any ideas or explanations for the lack of replicating in phase III? Were there different inclusion criteria? Was it differences in the patient population that might explain why we couldn’t get those really impressive returns in the phase III program?”
The phase II results showed no clear dose-response relationship with sozinibercept. “There were two different doses of sozinibercept in phase II, and one of them showed a very robust, superior outcome,” said Wykoff. “The other arm showed equivalence to ranibizumab, no dose response. Maybe that was a signal looking back.”
Khurana noted that the phase III trial design deviated from phase II by excluding patients with retinal angiomatous proliferation (RAP) lesions. Wykoff said the change was minor, affecting about 10% of patients who would have been eligible in the phase II study.
“The last point is that patients with superior outcomes with combination therapy in phase II did remarkably well,” Wykoff continued. “They gained 16 letters, on average. In phase III, the best-performing arm gained 13 letters. If I had to put my finger on [a reason for the conflicting data], I would say the phase II combination arm was an outlier.”
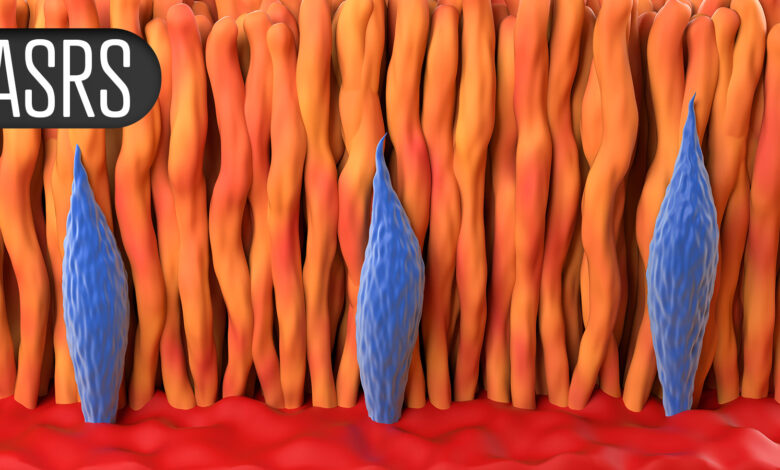
Both animal models and human data support a role for alternative VEGF family members in nAMD pathogenesis. An inhibitor of VEGF C and D, sozinibercept was designed for use in combination with VEGF-A inhibitors. The favorable outcome of a phase II trial provided impetus for the phase III COAST trial (which Wykoff reported) and the similarly designed ShORe trial.
COAST investigators enrolled patients with active choroidal neovascularization >50 lesion, including classic, minimally classic, and occult lesions. Eligible patents also had baseline BCVA of 25-60 letters. The patients were randomized to three treatment groups: aflibercept paired with two dosing schedules of sozinibercept or aflibercept plus sozinibercept sham injections. The primary endpoint was mean change in BCVA at 52 weeks.
Data analysis included a total of 993 patients. The results showed a small numerical difference in favor of aflibercept, but the difference did not achieve statistical significance versus either of the combination arms. The proportion of patients gaining ≥15 letters in BCVA ranged between 51.5% and 52.2%, and the proportion gaining ≥10 letters ranged from 64.4% to 66.1%. Mean reductions in CST ranged from 149.36-155.29 µm across the three treatment groups. The mean CNV regression was 4.61 mm2 with aflibercept alone and 4.91 and 4.92 mm2 in the two combination arms.
Rates of treatment-emergent adverse events (TEAEs) and serious TEAEs were similar across the treatment groups. TEAE-associated discontinuation rates were 2.1% with aflibercept alone versus 2.7% and 4.5% in the combination arms. One case of ocular inflammation occurred with aflibercept monotherapy as compared with three in one combination arm and none in the other.
Results from ShORe were similar. Mean improvement in BCVA after 52 weeks was 14.23 letters with aflibercept alone versus 12.68 and 13.14 letters in the combination arms. Mean reductions in CST were 144.29 µm with aflibercept alone and 149.75 and 166.83, respectively, in the two combination arms.
Disclosures
The COAST and ShORe studies were supported by Opthea. Some co-authors are company employees.
Wykoff disclosed multiple relationships with industry including Opthea.
Khurana disclosed relationships with Apellis, Annexion, Bausch, Genentech, Roche, RegenXBio, Clearside, AbbVie, Alcon, Regeneron, and Opthea.
Primary Source
American Society of Retina Specialists
Source Reference: Wykoff CC, et al “COAST: A phase III study of intravitreal sozinibercept combined with aflibercept in participants with neovascular age-related macular degeneration” ASRS 2025.



