NFL head coach, GM interview tracker: Falcons to interview Bill Belichick, Jim Harbaugh a second time
The latest news, rumors and updates for NFL coaching changes and searches
With the NFL regular season behind us, it is time for teams to begin preparing for next season. Several teams have already made the decision to change key positions within the organization, whether that be a general manager, head coach or coordinator.
Rather than scouring the scatter shot reports across social media, CBSSports.com has compiled all of those reports of interest in one place. Below, we will track all of the coordinator, head coach and general manager candidates and where they have been requested to interview.
Head coaches
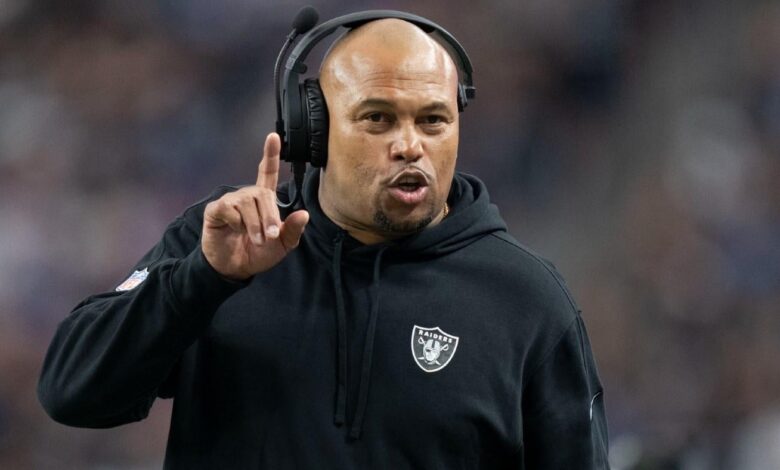
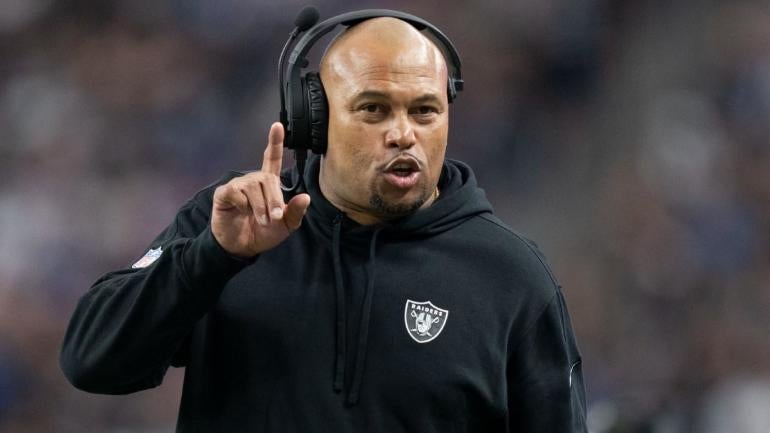
Las Vegas Raiders, HIRED Antonio Pierce
The Las Vegas Raiders are sticking with their interim head coach and hiring Antonio Pierce, according to CBS Sports NFL Lead Insider Jonathan Jones. Pierce replaced Josh McDaniels and went 5-4 down the stretch in Las Vegas.
New England Patriots: HIRED Jerod Mayo
In what was rumored to be happening for days, really weeks, Bill Belichick and the Patriots parted ways last Thursday. The next morning, the Patriots executed their succession plan by hiring linebackers coach Jerod Mayo to replace Belichick.
Atlanta Falcons
The Falcons parted ways with Arthur Smith after three losing seasons. The season-ending defeat to New Orleans capped Atlanta’s third consecutive 7-10 season under Smith, who was hired away from the Tennessee Titans prior to the 2021 campaign. Here are the candidates the Falcons have requested to interview:
- Bill Belichick, former Patriots HC (CBS Sports Lead NFL Insider Jonathan Jones) — second interview
- Jim Harbaugh, Michigan HC (NFL Media) — second interview
- Ben Johnson, Lions OC (CBS Sports Lead NFL Insider Jonathan Jones)
- Bobby Slowik, Texans OC (The MMQB)
- Mike Vrabel, former Titans HC (CBS Sports Lead NFL Insider Jonathan Jones)
- Brian Callahan, Bengals OC (Team) — completed
- Ejiro Evero, Panthers DC (Team) — completed
- Steve Wilks, 49ers DC (Team) — completed
- Anthony Weaver, Ravens DL coach (Team) — completed
- Mike Macdonald, Ravens DC (Team) — completed
- Aaron Glenn, Lions DC (Team) — completed
- Brian Johnson, Eagles OC (Team) — completed
- Raheem Morris, Rams DC (Team) — completed
Antonio Pierce, Raiders interim HC (NFL Network)
Carolina Panthers
After replacing Matt Rhule as the head coach in Carolina, Frank Reich lasted less than one full season with the Panthers. Owner David Tepper pulled the plug on the union after the team opened the season with a 1-10 record. Special teams coach Chris Tabor was promoted to the interim. Here are the candidates the Panthers have requested to interview:
- Ben Johnson, Lions OC (CBS Sports Lead NFL Insider Jonathan Jones)
- Todd Monken, Ravens OC (CBS Sports Lead NFL Insider Jonathan Jones)
- Dave Canales, Buccaneers OC (NFL Media)
- Bobby Slowik, Texans OC (CBS Sports Lead NFL Insider Jonathan Jones)
- Mike Macdonald, Ravens DC (The Athletic)
- Frank Smith, Dolphins OC (The Athletic)
- Brian Johnson, Eagles OC (ESPN)
- Dan Quinn, Cowboys DC (Team) — completed
- Raheem Morris, Rams DC (Team) — completed
- Brian Callahan, Bengals OC (Team) — completed
- Chris Tabor, Panthers interim head coach (Team)
- Ejiro Evero, Panthers DC (Team)
Los Angeles Chargers
Former head coach Brandon Staley accumulated a 24-25 record, including 0-1 in the postseason in his two-plus seasons as head coach of the Chargers. Ownership elected to make a change Dec. 15 after the team started 5-9. Assistant coach Giff Smith was promoted in the interim. Here are the candidates the Chargers have requested to interview:
- Giff Smith, Chargers interim HC (CBS Sports Lead NFL Insider Jonathan Jones)
- Steve Wilks, 49ers DC (CBS Sports Lead NFL Insider Jonathan Jones)
- Todd Monken, Ravens OC (NFL Media)
- Ben Johnson, Lions OC (NFL Media)
- Patrick Graham, Raiders DC (NFL Media)
- Dan Quinn, Cowboys DC (NBC Sports)
- Patrick Graham, Raiders DC (NBC Sports)
- Raheem Morris, Rams DC (CBS Sports Lead NFL Insider Jonathan Jones)
- Brian Callahan, Bengals OC (NFL Media)
- Kellen Moore, Chargers OC (CBS Sports Lead NFL Insider Jonathan Jones)
- Leslie Frazier, former Bills DC (CBS Sports Lead NFL Insider Jonathan Jones)
- Jim Harbaugh, Michigan HC (NFL Media)
- Mike Vrabel, former Titans HC (CBS Sports Lead NFL Insider Jonathan Jones)
- David Shaw, former Stanford HC (ESPN)
- Mike Macdonald, Ravens DC (Team) — completed
- Aaron Glenn, Lions DC (Team) — completed
Seattle Seahawks
In a shocking move, Pete Carroll is out as Seahawks head coach, according to CBS Sports Lead NFL Insider Jonathan Jones. Carroll, the oldest coach in the NFL, signed a five-year contract extension in 2020. He finishes his career in Seattle with a regular-season record of 137-89-1 over 14 seasons. According to Seahawks chair Jody Allen, the team and Carroll mutually agree that he would transition into an advisory role moving forward. Here are the candidates the Seahawks have requested to interview:
- Ejiro Evero, Panthers OC (NFL Media)
- Dan Quinn, Cowboys OC (NFL Media)
- Frank Smith, Dolphins OC (NFL Media)
- Mike Kafka, Giants OC (The Athletic)
- Raheem Morris, Rams DC (CBS Sports Lead NFL Insider Jonathan Jones)
- Bobby Slowik, Texans OC (NFL Media)
- Ben Johnson, Lions OC (NFL Media)
- Patrick Graham, Raiders DC (NFL Media)
Tennessee Titans
The Titans fired Mike Vrabel after six seasons in Tennessee. The Titans are coming off back-to-back losing seasons and finished 6-11 and in last place in the AFC South. Vrabel reached the postseason in three of his first four seasons, winning back-to-back division titles in 2020 and 2021. He reached the AFC title game in 2019 and compiled a 54-45 overall record. Here are the candidates the Titans have requested to interview:
- Aaron Glenn, Lions DC (ESPN)
- Brian Callahan, Bengals OC (NFL Media)
- Ben Johnson, Lions OC (CBS Sports NFL Lead Insider Jonathan Jones)
- Mike Kafka, Giants OC (CBS Sports NFL Lead Insider Jonathan Jones)
- Mike Macdonald, Ravens DC (ESPN)
- Dan Quinn, Cowboys DC (NFL Media)
- Bobby Slowik, Texans OC (NFL Media)
- Brian Johnson, Eagles OC (NFL Media)
- Thomas Brown, Panthers OC (ESPN)
- David Shaw, former Stanford HC (ESPN)
Antonio Pierce, Raiders former interim HC (NFL Media)
Washington Commanders
Ron Rivera went 26-40-1 over four seasons as Washington’s head man, but he was dismissed the day after the Commanders’ Week 18 loss to Dallas, setting the stage for a sweeping offseason overhaul under a new ownership group led by Josh Harris. Here’s a look at who the Commanders have requested to interview:
- Ben Johnson, Lions OC (NFL Media)
- Aaron Glenn, Lions DC (NFL Media)
- Raheem Morris, Rams DC (CBS Sports Lead NFL Insider Jonathan Jones)
- Anthony Weaver, Ravens associate HC and DL coach (ESPN)
- Mike Macdonald, Ravens DC (CBS Sports HQ Senior NFL Insider Josina Anderson)
- Dan Quinn, Cowboys DC (via NFL Media)
- Bobby Slowik, Texans OC (The Washington Post)
General managers
Washington Commanders: HIRED Adam Peters
CBS Sports Lead NFL Insider Jonathan Jones reported Friday that Washington had hired Adam Peters as its new GM.
Carolina Panthers
The Panthers fired general manager Scott Fitterer Monday, two months after the franchise dismissed Frank Reich as head coach. Here are all the general manager interview candidates the Panthers asked for permission to interview, per the team.
- Brandon Brown, Giants assistant general manager
- Ed Dodds, Colts assistant general manager
- Mike Greenberg, Buccaneers assistant general manager
- Alec Halaby, Eagles assistant general manager
- Khai Harley, Saints vice president of football administration
- Champ Kelly, Raiders interim general manager
- Nick Matteo, Ravens vice president of football administration
- Brandt Tilis, Chiefs vice president of football operations
- Dan Morgan, Panthers assistant GM
- Mike Disner, Lions COO
- Samir Suleiman, Panthers vice president of football administration
Las Vegas Raiders
The Raiders have hired head coach Antonio Pierce, but they’re still looking for a general manager. Champ Kelly served as the interim GM this past season.
Los Angeles Chargers
In addition to parting ways with head coach Brandon Staley, they moved on from general manager Tom Telesco, who had served in the role for nearly 11 full seasons. He was with the organization through the move from San Diego. JoJo Wooden was named interim general manager.
- JoJo Wooden, Chargers interim GM (CBS Sports Lead NFL Insider Jonathan Jones)
- Brandon Brown, Giants assistant general manager (NFL Media)
- Terrance Gray, Bills director of player personnel (NFL Media)
- Ian Cunningham, Bears assistant general manager (NFL Media)
- Jeff Ireland, Saints vice president and assistant general manager for college personnel (NFL Media)
- Joe Hortiz, Ravens director of player personnel (CBS Sports Lead NFL Insider Jonathan Jones)
New England Patriots
Since Bill Belichick also ran football operations, the Patriots are currently looking for a new GM after replacing Belichick with Jerod Mayo as head coach.




