Guillain-Barre Syndrome Rates After RSV Shots in Sync With Trial Data, CDC Says
—
But compared with mRNA COVID-19 vaccines, GBS was more common than expected
by
Katherine Kahn,
Staff Writer, MedPage Today
May 31, 2024
Reports of Guillain-Barré syndrome (GBS) following respiratory syncytial virus (RSV) vaccination in adults ages 60 and up were higher than expected, but the vaccine’s benefits still outweigh any small potential risk, according to a new CDC analysis.
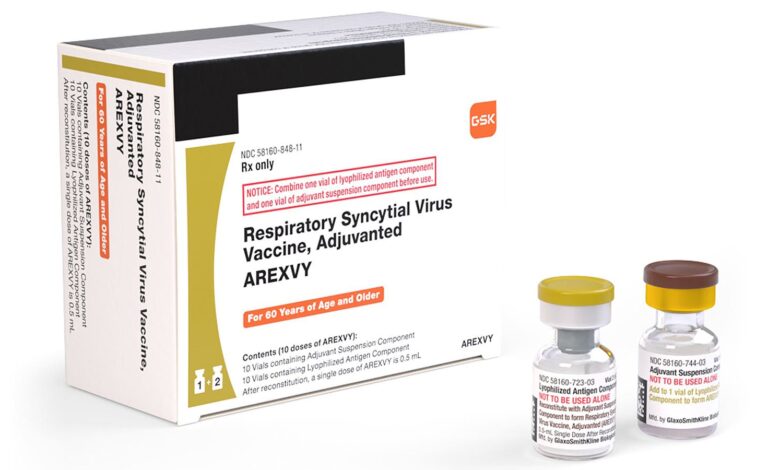
Data from the Vaccine Adverse Event Reporting System (VAERS) revealed that there were 1.5 reports of GBS per 1 million doses administered of the GSK RSV vaccine (Arexvy), and 5 reports per 1 million doses administered of the Pfizer RSV vaccine (Abrysvo), according to researchers led by Anne Hause, PhD, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases in the Morbidity and Mortality Weekly Report.
“Using the reporting rate for mRNA COVID-19 vaccines as an estimate of background rate, reports of GBS after RSV vaccination were more common than expected,” the CDC authors wrote, though VAERS data generally cannot determine causal associations between adverse events and vaccinations, they pointed out.
Of a total of 28 cases of GBS in older adults after RSV vaccination that were reported to VAERS from May 2023 to mid-April 2024, 60.3% occurred after receipt of the Pfizer RSV vaccine and 39.3% after the GSK vaccine.
There were two fatalities associated with GBS out of a total of 18 reported deaths from a variety of reasons.
To put these numbers into context, at least 10.6 million adults ages 60 and older received an RSV shot from August 2023, when the newly approved GSK and Pfizer vaccines were being rolled out, to the end of March 2024.
During prelicensure clinical trials, GBS was identified as a potential safety concern, and the rates of GBS after RSV vaccination are in general alignment with what was observed in clinical trials of the vaccines, the authors wrote. CDC officials announced at a February 2024 meeting of the Advisory Committee on Immunization Safety that they were monitoring the situation.
Researchers used the VAERS reporting rates of GBS for mRNA COVID-19 vaccines to provide an estimate of background rates of GBS in people ages 60 and up. Previously the Vaccine Safety Datalink surveillance program had found no increased risk for GBS after vaccination with mRNA COVID-19 vaccines, they noted.
From early May 2023 to mid-April 2024, VAERS processed 3,200 adverse event reports among people 60 years and older (median age 72 years) who reported RSV vaccination. About 70% of reported adverse events occurred in women. Among the reports, 68.5% were related to the GSK vaccine and 28.8% to the Pfizer vaccine.
The most commonly reported events were extremity pain, headache, injection site pain, and fatigue; most (91.2%) were considered non-serious. Of the 8.8% that were considered serious, about 7% of the reports were for hospitalization, 2.5% for life-threatening illness, 2.1% for permanent disability, and 1.1% for death.
Reported causes of death, other than the two cases of GBS, included severe respiratory illness and failure, cardiovascular events, hepatic encephalopathy, RSV infection, and sepsis, among others.
Researchers also looked at adverse event reports from V-safe , another CDC surveillance system for the general public that was initially developed to monitor the safety of COVID-19 vaccines and, subsequently, the RSV vaccines.
From V-safe data, researchers found that among the 16,220 people ages 60 years and older, 39.5% reported receiving the GSK vaccine and 23.9% received the Pfizer vaccine. The remainder did not know the manufacturer of the vaccine. About 31% reported receiving multiple vaccines during the same visit, most commonly the COVID-19 and influenza vaccines.
The most frequently reported symptoms were injection site reactions, fatigue, and muscle and body aches. Most reported that symptoms were mild to moderate in severity. However, in the week after vaccination, about 8% of vaccine recipients reported being unable to perform normal daily activities, but only 0.4% sought medical care for those symptoms.
Hause and colleagues pointed out several limitations of the report. VAERS may be subject to reporting biases and V-safe is a voluntary program and may not be representative of the vaccinated population. Also the data do not include a comparator group of unvaccinated people, so estimating the magnitude of risk for GBS after vaccination is not possible.
The CDC continues to conduct active safety evaluations to assess GBS risk and other adverse events that are reported after RSV vaccination, and will use that information to guide future vaccine recommendations. However, RSV vaccination continues to be recommended in adults ages 60 and up, in the context of shared clinical decision-making.
-
![author['full_name']](https://assets.medpagetoday.net/media/images/author/2N5A0622_180.jpg)
Katherine Kahn is a staff writer at MedPage Today, covering the infectious diseases beat. She has been a medical writer for over 15 years.
Disclosures
Hause and other study authors reported no relevant financial disclosures.
Primary Source
Morbidity and Mortality Weekly Report
Source Reference: Hause AM, et al “Early safety findings among persons aged ≥60 years who received a respiratory syncytial virus vaccine — United States, May 3, 2023-April 14, 2024” MMWR 2024; DOI: 10.15585/mmwr.mm7321a3.


