Intravascular Imaging-Guided PCI Reaches a Turning Point With Survival, MI Benefits
— Updated meta-analysis provides strong impetus for IVUS, OCT adoption
by
Nicole Lou, Senior Staff Writer, MedPage Today
February 21, 2024
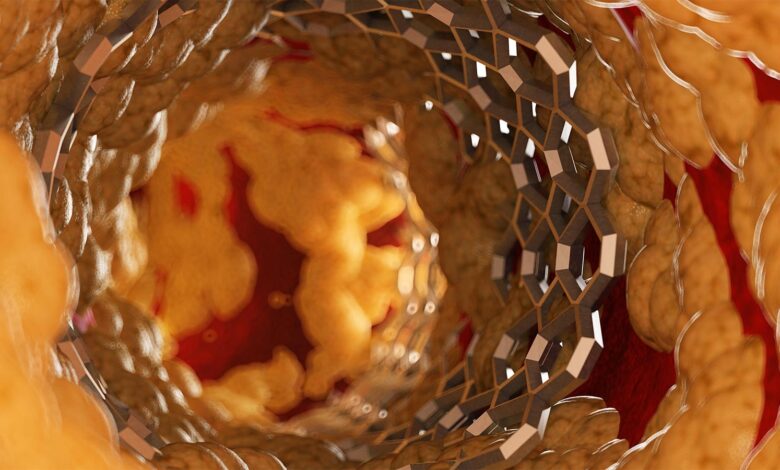
For the first time, intravascular imaging-guided coronary stenting was associated with better survival and reduced myocardial infarction (MI) in a meta-analysis powered to detect these benefits against angiography, researchers reported.
Randomized to optical coherence tomography (OCT) or intravascular ultrasound (IVUS) guidance, patients who underwent percutaneous coronary intervention (PCI) with contemporary stents showed a decrease in target lesion failure (RR 0.71, 95% CI 0.63-0.80) and its individual endpoint components of:
- Cardiac death: RR 0.55 (95% CI 0.41-0.75)
- Target vessel MI: RR 0.82 (95% CI 0.68-0.98)
- Target lesion revascularization: RR 0.72 (95% CI 0.60-0.86)
Additionally, the two intravascular imaging modalities were tied to decreases in stent thrombosis (RR 0.52, 95% CI 0.34-0.81), all MI (RR 0.83, 95% CI 0.71-0.99), and all-cause death (RR 0.75, 95% CI 0.60-0.93) when participants were followed for a weighted average of 24.7 months, reported a group led by Gregg Stone, MD, of Icahn School of Medicine at Mount Sinai in New York City.
“Compared with angiography guidance, intravascular imaging guidance of coronary stent implantation with OCT or intravascular ultrasound enhances both the safety and effectiveness of PCI,” the authors concluded in The Lancet.
“To place these results in perspective, drug-eluting stents [DES] do not reduce death, myocardial infarction, or stent thrombosis compared with bare metal stents, yet are recommended with class I evidence in societal guidelines for their reduction in repeat revascularization alone,” they wrote.
Meanwhile, IVUS and OCT imaging are still stuck with a weak class IIa endorsement from societal guidelines on coronary revascularization despite older evidence that they reduce composite cardiac events and repeat revascularization compared with angiographic guidance alone.
“In contrast to the plateau in clinical outcomes that has been reached with drug-eluting stent technology, event-free survival might still be substantially improved by implanting drug-eluting stents with intravascular imaging guidance,” Stone and colleagues stressed.
The study authors suggested greater adoption of IVUS and OCT in mainstream clinical practice based on the meta-analysis. “These data warrant efforts to overcome remaining impediments to the routine use of intravascular imaging, including training and reimbursement issues,” Stone’s group urged.
Zhong Shiun Lee, MBBS, and Nicola Ryan, MBBCh, MPH, both of Aberdeen Royal Infirmary in Scotland, agreed.
“To date, the question among clinical interventional cardiologists often revolves around when intravascular imaging should be used to guide PCI,” they wrote in an accompanying editorial. “[F]ollowing this meta-analysis the question surely becomes why are we not using intravascular imaging to guide PCI?”
“Substantial consideration to upgrading the use of intravascular imaging to a class I recommendation in future guidelines should occur as a result of the increased procedural safety and efficacy with the use of intravascular imaging demonstrated by this meta-analysis,” according to the editorialists.
Stone and colleagues had been motivated to perform their meta-analysis following the wave of positive IVUS/OCT trials released last summer, namely GUIDE-DES, ILUMIEN IV, OCTOBER, and OCTIVUS.
Ultimately, the researchers pooled 22 randomized trials published from 2010 to 2023. Included were nearly 16,000 patients undergoing PCI with DES randomized either to IVUS/OCT or to angiography alone to guide the intervention. Patients represented a range of clinical presentations and coronary anatomy complexity.
No differences in outcomes between IVUS and OCT groups could be detected by the sample.
Stone’s group reported that their results comparing intravascular imaging against angiography were generally supported by a separate network meta-analysis relying on indirect data and overall treatment effects.
“Between-study heterogeneity was minimal or absent for all endpoints examined in each pairwise comparison, publication bias was not detected, no areas of inconsistency were noted within the network, and the direct and indirect data were consistent for each comparison within the network. Analysis with Bayesian and frequentist methods also provided similar treatment effect estimates,” the authors added.
Nevertheless, the meta-analysis was limited by differences in individual trial designs and protocols that could not be adjusted for with individual patient-level data. The report was also not designed to determine how mechanistically IVUS and OCT could produce benefits in hard clinical outcomes, nor to assess complications attributed to intravascular imaging catheters.
“Finally, optimal imaging criteria differed between trials, making it impossible to draw conclusions with regard to which criteria should be used in clinical practice,” Lee and Ryan commented.
“Additional investigation is required to determine which patient and lesion types benefit most from intravascular imaging guidance and to establish the optimal techniques and procedural objectives for OCT-guided and [IVUS]-guided stent implantation,” study authors acknowledged.
-
![author['full_name']](https://clf1.medpagetoday.com/media/images/author/nicoleLou_188.jpg)
Nicole Lou is a reporter for MedPage Today, where she covers cardiology news and other developments in medicine. Follow
Disclosures
The study was funded by Abbott.
Stone declared receiving speaker honoraria from Medtronic, Pulnovo, Infraredx, Abiomed, Amgen, and Boehringer Ingelheim; consulting to Abbott, Daiichi Sankyo, Ablative Solutions, CorFlow, Apollo Therapeutics, Cardiomech, Gore, Robocath, Miracor, Vectorious, Abiomed, Valfix, TherOx, HeartFlow, Neovasc, Ancora, Elucid Bio, Occlutech, Impulse Dynamics, Adona Medical, Millennia Biopharma, Oxitope, Cardiac Success, and HighLife; and holding equity or options from Ancora, Cagent, Applied Therapeutics, the Biostar family of funds, SpectraWave, Orchestra BioMed, Aria, Cardiac Success, Valfix, and Xenter. Stone’s institution also receives research grants from Abbott, Abiomed, BioVentrix, Cardiovascular Systems, Phillips, Biosense-Webster, Shockwave, Vascular Dynamics, Pulnovo, and V-wave.
Co-authors have multiple relationships with industry.
Lee reported speakers’ fees from AstraZeneca, Biosensors International, and Novartis.
Ryan disclosed speakers’ fees from Abbott.
Primary Source
The Lancet
Source Reference: Stone GW, et al “Intravascular imaging-guided coronary drug-eluting stent implantation: an updated network meta-analysis” Lancet 2024; DOI: 10.1016/S0140-6736(23)02454-6.
Secondary Source
The Lancet
Source Reference: Lee ZS, Ryan N “Intravascular imaging in percutaneous coronary intervention” Lancet 2024; DOI: 10.1016/S0140-6736(23)02686-7.

