Telehealth offers convenience for rural patients—but at what cost?

Remote health care delivery, commonly known as telehealth or telemedicine, is often beneficial for patients who have difficulty visiting their preferred health care providers in person. Use of the technology was rising steadily in the years leading up to the COVID-19 pandemic and it has now become commonplace.
In a recent paper forthcoming in the Review of Financial Studies, Zihan Ye, assistant professor of finance at the University of Tennessee, Knoxville, Haslam College of Business, and co-authors Kimberly Cornaggia (Penn State University) and Xuelin Li (Columbia Business School) investigated the financial effects of telemedicine. Their research reveals that the convenient service may have unexpected consequences on patients‘ long-term access to acute care.
Redistribution of hospital operations and access to capital
Most remote health care delivery comes from urban hospitals, which are more likely than their rural counterparts to have the workforce, infrastructure and profit potential to provide such services. Technology enables rural patients to access these facilities’ often superior care without the expense and time commitment associated with travel.
Even when rural patients receive local in-person care, such as surgery, many still opt for telehealth services from urban providers for initial consultations and recovery monitoring.
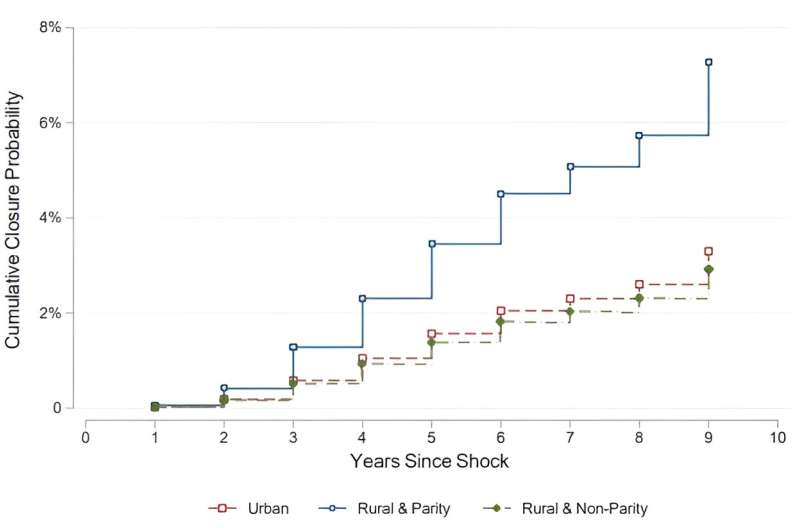
However, telemedicine usage can have a surprising impact on rural communities’ access to local care. By analyzing data from medical claims and hospital financial statements, Ye and her colleagues found that rural health care providers lose patients to urban hospitals that offer telehealth.
In turn, this loss negatively impacts rural hospitals, influencing their investment decisions and capital structure, and leading to the divestment of physicians, nurses and intensive care units.
“Rural hospitals are losing, on average, a lot of money,” Ye says. “There are more bankruptcies of rural hospitals than urban ones. Local governments and authorities are trying hard to protect them so local patients can have access to health care providers. From a policy perspective, there should be more collaboration programs where the rural hospitals can get a share from this telehealth provision so they do not end up in bankruptcy.”
Telehealth demand drives price wars
By offering remote health care delivery, hospitals can increase demand for their services. Telemedicine provides patients with more choices, intensifying competition among hospitals and often leading to a price war, with urban hospitals typically charging more than their rural counterparts.
Rural hospitals, which do not benefit as much from an influx of additional patients, generally do not adopt telehealth services. As a result, these rural facilities attract fewer patients and face indirect price reductions.
Insurance reimbursement also influences hospitals’ decisions to offer telehealth services. Health care facilities treating a significant number of Medicare and Medicaid patients face a reimbursement risk.
“Medicare and Medicaid are known for under-reimbursement, so when hospitals take those patients, they might not get reimbursed as much compared to commercial insurances,” says Ye.
Downgraded credit ratings and higher yield requirements
Since urban health care facilities receive most of the revenue generated by telehealth services, rural hospitals face lower net income and profit margins. This financial strain leads to higher leverage and results in downgraded credit ratings for bonds issued by these rural hospitals.
“Bond repayment depends on the issuer’s future cash flows, so when rural hospitals lose patients to urban ones and their cash flow starts to deteriorate, investors face higher risk and require higher yield,” Ye says. “So now when the rural hospitals issue bonds, they will have to offer a higher yield, and that translates into a financial burden for them.”
While patients choose remote health care primarily because of convenient access to superior care, Ye says these patients should consider long-term financial ramifications, as should policymakers who have the power to influence which providers can afford to offer telemedicine at all.
“As communication technology now impacts all of our lives, we should be aware of the consequences that come with it,” Ye says. “When patients are getting access to better health care through telehealth, they should also be aware of the potential negative spillovers to rural hospitals and rural patients.”
More information:
Cornaggia, Kimberly and Li, Xuelin and Ye, Zihan, Financial Effects of Remote Product Delivery: Evidence from Hospitals (October 25, 2023). Review of Financial Studies, forthcoming, Available at SSRN: ssrn.com/abstract=3833193
Citation:
Telehealth offers convenience for rural patients—but at what cost? (2024, August 1)
retrieved 1 August 2024
from https://medicalxpress.com/news/2024-08-telehealth-convenience-rural-patients.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.



